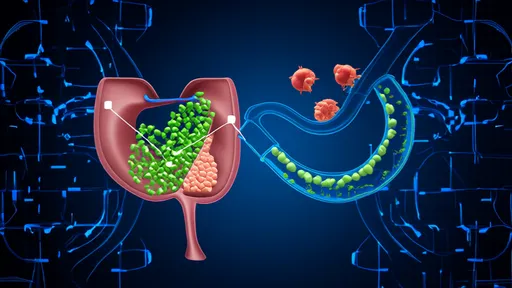
Non-alcoholic fatty liver disease (NAFLD) has quietly become one of the most prevalent chronic liver conditions worldwide, affecting approximately 25% of the global population. Unlike liver damage caused by excessive alcohol consumption, NAFLD stems from metabolic dysfunction and is intricately linked to poor dietary habits. The condition ranges from simple steatosis (fat accumulation in liver cells) to more severe forms like non-alcoholic steatohepatitis (NASH), which can progress to cirrhosis and liver failure. What makes NAFLD particularly insidious is its asymptomatic nature in early stages, often going undetected until significant liver damage has occurred.
The Western Diet: A Perfect Storm for NAFLD
Modern dietary patterns characterized by excessive consumption of processed foods, refined carbohydrates, and sugary beverages have created an ideal environment for NAFLD to flourish. The typical Western diet, high in fructose and saturated fats, directly contributes to hepatic fat accumulation and insulin resistance – two key drivers of NAFLD pathogenesis. Fructose, particularly from high-fructose corn syrup found in countless processed foods and drinks, is metabolized differently than glucose, bypassing regulatory pathways and overwhelming the liver's capacity to process it effectively.
Emerging research suggests that it's not just about the quantity of food but the quality and composition of our diet that significantly impacts NAFLD progression. The Mediterranean diet, rich in monounsaturated fats, omega-3 fatty acids, and polyphenol-rich plant foods, has shown remarkable protective effects against NAFLD development and progression. This dietary pattern emphasizes extra virgin olive oil as the primary fat source, abundant consumption of vegetables and fruits, moderate intake of fish and poultry, and limited red meat and processed foods.
The Sugar Paradox: Sweet Poison for the Liver
While fat has traditionally been blamed for fatty liver, sugar – particularly in liquid form – appears to be an even greater culprit. Soft drinks and fruit juices deliver massive fructose loads directly to the liver without the fiber that would normally slow absorption in whole fruits. This fructose flood triggers de novo lipogenesis, the process by which the liver converts excess carbohydrates into fat. Regular consumption of sugar-sweetened beverages has been strongly associated with increased liver fat content, independent of total calorie intake or body weight.
Artificial sweeteners, once thought to be a safe alternative, may not be the solution either. Recent studies indicate that non-caloric sweeteners can alter gut microbiota in ways that promote glucose intolerance and may paradoxically contribute to metabolic dysfunction. This revelation has led researchers to reconsider dietary strategies for NAFLD, shifting focus from mere calorie reduction to comprehensive dietary pattern modification.
The Power of Macronutrient Composition
Beyond simply reducing calories, the specific macronutrient composition of the diet appears to play a crucial role in NAFLD management. Low-carbohydrate diets, particularly those emphasizing healthy fats and adequate protein, have demonstrated superior results in reducing liver fat compared to traditional low-fat diets. This challenges decades of dietary dogma that vilified all fats while giving carbohydrates a free pass. The ketogenic diet, an extremely low-carb approach, has shown promise in preliminary studies, though its long-term sustainability and effects require further investigation.
Protein quality matters as well. Plant-based proteins from legumes, nuts, and seeds may offer advantages over animal proteins for NAFLD patients, as they come packaged with fiber and beneficial phytochemicals. However, lean animal proteins like fish and poultry can certainly be part of a liver-healthy diet when consumed in moderation. The key lies in achieving the right balance while minimizing processed meats and high-fat dairy products.
Micronutrients: Small Compounds with Big Impact
Certain micronutrients have emerged as potential allies in the fight against NAFLD. Vitamin E, particularly in its natural form as mixed tocopherols, has demonstrated efficacy in reducing liver inflammation in non-diabetic patients with NASH. However, high-dose supplementation requires medical supervision due to potential risks. Polyphenols, abundant in colorful fruits, vegetables, tea, coffee, and dark chocolate, exert antioxidant and anti-inflammatory effects that may protect hepatocytes from damage.
Choline, an essential nutrient found in eggs, liver, and soybeans, plays a critical role in lipid metabolism and may help prevent excessive fat accumulation in the liver. Interestingly, coffee consumption has been consistently associated with reduced risk of NAFLD progression, possibly due to its chlorogenic acid content and other bioactive compounds. These findings highlight the importance of a nutrient-dense, whole foods approach rather than focusing on single nutrients in isolation.
The Gut-Liver Axis: Dietary Fiber as a Therapeutic Agent
Growing understanding of the gut-liver axis has revealed how gut microbiota composition influences NAFLD development and progression. Dietary fiber, particularly soluble fiber found in oats, legumes, and certain fruits, serves as fuel for beneficial gut bacteria that produce short-chain fatty acids (SCFAs). These SCFAs help maintain gut barrier integrity, reducing endotoxin translocation to the liver that can trigger inflammation. Fermentable fibers may also directly modulate hepatic fat metabolism through mechanisms involving gut hormone secretion.
Probiotic-rich foods like yogurt, kefir, and fermented vegetables may offer additional benefits by promoting a healthy gut microbiome. Preliminary studies suggest specific probiotic strains might help reduce liver fat and inflammation, though more research is needed to establish definitive recommendations. The synergy between prebiotic fibers and probiotic foods creates a gut environment that appears protective against NAFLD progression.
Practical Implementation: From Theory to Plate
Translating these scientific insights into practical dietary changes presents challenges in our modern food environment. A successful NAFLD dietary intervention must be culturally appropriate, economically feasible, and sustainable long-term. Simple swaps like replacing sugary drinks with water or herbal tea, choosing whole grains over refined carbohydrates, and increasing vegetable intake at each meal can yield significant benefits. Meal timing and eating patterns, such as time-restricted eating, may also influence NAFLD by aligning food intake with circadian rhythms and allowing for longer fasting periods that promote fat utilization.
Cooking methods matter too. Grilling, baking, or steaming foods preserves more nutrients and avoids the harmful compounds produced by deep-frying. Using herbs and spices not only enhances flavor without added salt but also provides additional bioactive compounds with potential liver-protective effects. Education about reading food labels to identify hidden sugars and unhealthy fats becomes an essential skill for NAFLD patients navigating the grocery store.
The Road Ahead: Personalized Nutrition for NAFLD
As research progresses, the field is moving toward more personalized dietary approaches for NAFLD management. Genetic variations, microbiome profiles, and metabolic characteristics may eventually guide tailored dietary recommendations. For now, the evidence consistently points to a whole-food, plant-predominant dietary pattern with careful attention to sugar and refined carbohydrate intake as the foundation for preventing and managing NAFLD. While pharmaceutical treatments for NAFLD remain limited, dietary intervention stands as the cornerstone of therapy – a powerful tool that patients can harness to take control of their liver health.
The battle against NAFLD begins at the dinner table. By making informed food choices and adopting sustainable eating patterns, individuals can significantly impact the course of this silent epidemic. Healthcare providers must prioritize dietary counseling as part of comprehensive NAFLD management, empowering patients with the knowledge and tools to nourish their livers back to health.
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025