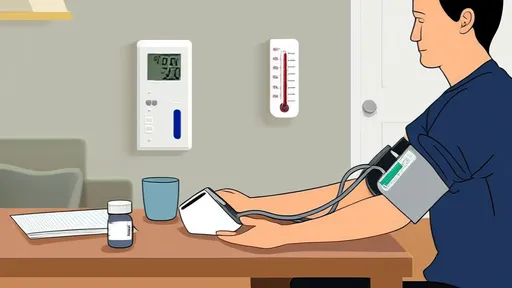
In an era where preventive healthcare is gaining prominence, home blood pressure monitoring has emerged as a critical tool for managing cardiovascular health. Unlike sporadic clinic readings, regular at-home measurements provide a more comprehensive picture of one's blood pressure patterns, free from the artificial spikes caused by white-coat hypertension. This practice empowers individuals to take an active role in their health management while providing physicians with valuable data for more accurate diagnoses and treatment adjustments.
Understanding the proper technique forms the foundation of reliable home monitoring. Many users unknowingly compromise their readings by improper cuff placement or body positioning. The cuff should always sit snugly on bare skin at heart level, with the arm supported on a flat surface. Feet must remain flat on the floor, and patients should refrain from talking or crossing legs during the measurement. These seemingly small details can create variations of 10-15 mmHg - enough to potentially mask hypertension or prompt unnecessary medication changes.
The timing and frequency of measurements significantly influence the clinical usefulness of the data. Most experts recommend taking readings twice daily - once in the morning before medication and again in the evening. Each session should consist of two or three measurements taken one minute apart. This approach captures the natural circadian rhythm of blood pressure while accounting for normal measurement variability. Patients starting new medications or those with unstable readings may need more frequent monitoring during adjustment periods.
Device selection remains one of the most overlooked aspects of home monitoring. Not all blood pressure monitors are created equal. Look for devices validated by organizations like the Association for the Advancement of Medical Instrumentation or the British Hypertension Society. Upper arm cuffs generally provide more reliable results than wrist models, though proper fit is crucial - an ill-fitting cuff can distort readings by up to 30 mmHg. Patients with larger arms should seek out appropriately sized cuffs rather than settling for standard sizes.
Environmental factors play a surprisingly significant role in blood pressure readings. Measurements taken within 30 minutes of smoking, caffeine consumption, or exercise may show artificially elevated numbers. Even mundane activities like watching stressful news programs or engaging in heated discussions can temporarily spike readings. Creating a consistent, quiet environment for monitoring helps establish baseline values that truly reflect cardiovascular status rather than momentary stressors.
Data recording and interpretation transform random measurements into clinically actionable information. Simply remembering numbers or occasionally jotting them down defeats the purpose of home monitoring. Maintain a structured log that includes the time, date, any unusual symptoms, and medication times. Many modern devices sync with smartphone apps that automatically organize readings and generate trend reports. These visual representations help both patients and doctors identify patterns that might otherwise go unnoticed in isolated readings.
The psychological aspect of home monitoring deserves careful consideration. Some patients become overly anxious about daily fluctuations, not realizing that blood pressure naturally varies throughout the day. This "monitoring anxiety" can itself elevate readings, creating a frustrating cycle. Education about normal variability helps prevent unnecessary stress. Conversely, others might ignore consistently high readings, assuming they'll improve on their own. Finding the balance between vigilance and obsession is key to successful long-term monitoring.
Perhaps most importantly, home readings should complement - not replace - professional medical care. Patients sometimes make dangerous adjustments to medications based on home data without consulting their physicians. Others might dismiss concerning patterns, assuming their doctor would have said something during the last visit. Establishing clear communication protocols with healthcare providers ensures that home monitoring enhances rather than disrupts proper medical supervision.
As technology advances, the potential of home blood pressure monitoring continues to expand. Wireless devices that transmit data directly to electronic health records, sophisticated algorithms that detect irregular patterns, and integration with other health metrics all point toward a future where patients and doctors collaborate more effectively than ever in managing cardiovascular health. By mastering these fundamental principles today, individuals position themselves to benefit fully from these emerging innovations tomorrow.
The journey toward better blood pressure control begins not in the doctor's office, but in the daily choices made at home. With proper technique, appropriate equipment, and thoughtful interpretation, home monitoring becomes more than just numbers on a screen - it transforms into a powerful dialogue between patient and provider, a early warning system for potential problems, and most importantly, a pathway to lasting cardiovascular health.
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025