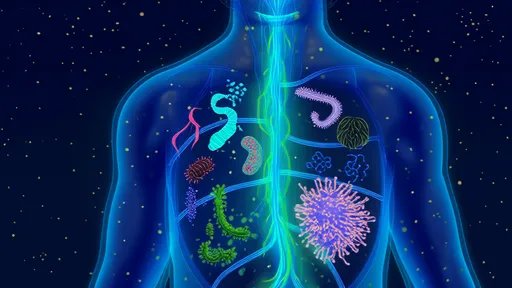
The human mouth is a bustling ecosystem teeming with microorganisms, collectively known as the oral microbiome. Far from being isolated to the confines of our gums and teeth, these microbial communities wield surprising influence over our overall health. Recent research has unveiled intricate connections between oral bacteria and systemic conditions, ranging from cardiovascular disease to diabetes and even Alzheimer’s. The mouth, it seems, is a window into the body’s wellbeing—or lack thereof.
The oral microbiome is a complex and dynamic environment. Comprising over 700 species of bacteria, viruses, fungi, and other microbes, it is second only to the gut in terms of microbial diversity. Under healthy conditions, these microorganisms coexist harmoniously, contributing to processes like digestion and immune defense. However, disruptions in this delicate balance—often caused by poor oral hygiene, smoking, or diet—can lead to dysbiosis, a state where harmful bacteria gain the upper hand. This shift doesn’t just cause cavities or gum disease; it can have far-reaching consequences for the entire body.
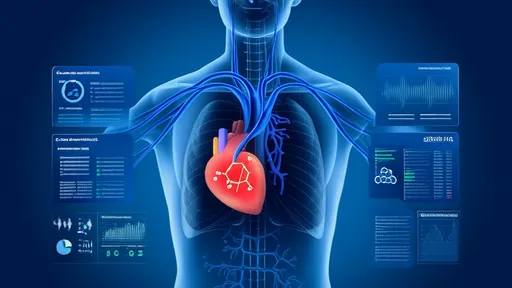
One of the most well-documented links is between oral health and cardiovascular disease. Studies have shown that bacteria like Porphyromonas gingivalis, a key player in periodontitis, can enter the bloodstream through inflamed gums. Once in circulation, these pathogens may contribute to the formation of arterial plaques, increasing the risk of heart attacks and strokes. Inflammation, a common thread in both gum disease and atherosclerosis, appears to amplify this connection. The evidence is compelling enough that some cardiologists now recommend periodontal screenings for patients with heart conditions.
Diabetes presents another striking example of the mouth-body connection. Individuals with diabetes are more prone to severe gum disease, and conversely, chronic periodontal inflammation can worsen blood sugar control. This bidirectional relationship creates a vicious cycle: high glucose levels feed harmful oral bacteria, while gum infections make diabetes harder to manage. Researchers speculate that the inflammatory molecules released by infected gums interfere with insulin sensitivity, further complicating metabolic regulation.
Emerging research has even implicated oral bacteria in neurodegenerative diseases like Alzheimer’s. Scientists have found traces of P. gingivalis in the brains of Alzheimer’s patients, along with elevated levels of enzymes produced by the bacterium. These enzymes, known as gingipains, are thought to damage neurons and exacerbate the accumulation of amyloid plaques—a hallmark of the disease. While the exact mechanisms remain under investigation, the findings suggest that maintaining oral health could be a modifiable risk factor in cognitive decline.
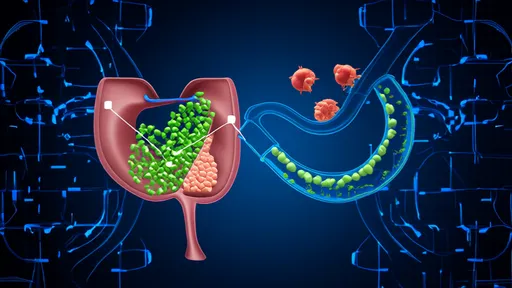
The gut microbiome, long a focus of systemic health research, also interacts with its oral counterpart. Swallowed saliva carries oral bacteria into the digestive tract, where they can influence gut microbial composition. Some studies suggest that certain oral pathogens may colonize the gut, potentially contributing to conditions like irritable bowel syndrome (IBS) or colorectal cancer. This gut-mouth axis underscores the importance of oral hygiene as part of a holistic approach to health.
Pregnancy introduces yet another dimension to the oral-systemic health link. Hormonal changes during pregnancy can make gums more susceptible to inflammation and infection, a condition known as pregnancy gingivitis. Worse, severe periodontal disease has been associated with preterm birth and low birth weight. Researchers believe that oral bacteria or their byproducts may trigger inflammatory responses that disrupt fetal development. For expectant mothers, this makes dental care not just a personal priority, but a critical factor in prenatal health.
Despite these alarming connections, there’s reason for optimism. Simple, consistent oral hygiene practices—brushing, flossing, and regular dental checkups—can significantly reduce the risk of dysbiosis and its systemic repercussions. Diet also plays a pivotal role; reducing sugar intake starves harmful bacteria, while fiber-rich foods promote a balanced microbiome. For those with existing conditions like diabetes or heart disease, collaboration between medical and dental professionals could lead to more comprehensive care strategies.
The science is clear: the mouth is not an isolated compartment but an integral part of our overall health landscape. As research continues to unravel the intricate dialogues between oral microbes and distant organs, one message rings true—taking care of our teeth and gums is an investment in far more than just a sparkling smile.
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025